Surgeries
Previous surgery, radiation therapy, infection and endometriosis can often cause significant scarring or adhesions in the pelvic tissues making pelvic surgery more complex. Injury to surrounding anatomic structures is a more common complication when there is scarring present. Surgeons need specialty training and should have experience in performing these more challenging surgeries to minimize the risks of damage to surrounding tissue.

Laparoscopy is performed under general anesthetic, so you will be unconscious throughout the procedure and have no memory of it. You can often go home on the same day.
During laparoscopy, the surgeon will make a small cut (incision) of around 1-1.5cm (0.4-0.6 inches), which is usually placed near your belly button.
A tube is inserted through the incision, and carbon dioxide gas is pumped through the tube to inflate your tummy (abdomen). Inflating your abdomen allows the surgeon to see your organs more clearly and gives them more room to work. A laparoscope is then inserted through this tube. The laparoscope will relay images to a television monitor in the operating theatre, giving the surgeon a clear view of the whole area.
If the laparoscopy is used to carry out a surgical treatment, such as removing your uterus or ovary, further incisions will be made in your abdomen. Small, surgical instruments can be inserted through these incisions, and the surgeon can guide them to the right place using the view from the laparoscope. Once in place, the instruments can be used to carry out the required treatment.
After the procedure, the carbon dioxide is let out of your abdomen, the incisions are closed using stitches or clips and a dressing is applied.
When laparoscopy is used to diagnose a condition, the procedure usually takes 30-60 minutes. It will take longer if the surgeon is treating a condition, depending on the type of surgery being carried out.
Exploratory laparotomy is done while you are under general anesthesia. This means you are asleep and feel no pain. Laparotomy is often the most invasive type of surgery but for many patients it is the most effective way of ensuring removal of the most amount of disease possible.
The surgeon makes a cut into the abdomen and examines the abdominal organs. The size and location of the surgical cut depends on the specific health concern.
EXPLORATORY LAPAROTOMY MAY BE USED TO HELP DIAGNOSE AND TREAT MANY HEALTH CONDITIONS, INCLUDING:
- Cancer of the ovary, colon, pancreas, liver
- Endometriosis
- Gallstones
- Hole in the intestine (intestinal perforation)
- Inflammation of the appendix (acute appendicitis)
- Inflammation of an intestinal pocket (diverticulitis)
- Inflammation of the pancreas (acute or chronic pancreatitis)
- Liver abscess
- Pockets of infection (retroperitoneal abscess, abdominal abscess, pelvic abscess)
- Pregnancy outside of the uterus (ectopic pregnancy)
- Scar tissue in the abdomen (adhesions)
Surgery is the main treatment for most ovarian cancers. How much surgery you have depends on how far your cancer has spread and on your general health. For women of childbearing age who have certain kinds of tumors and whose cancer is in the earliest stage, it may be possible to treat the disease without removing both ovaries and the uterus.
STAGING EPITHELIAL OVARIAN CANCER
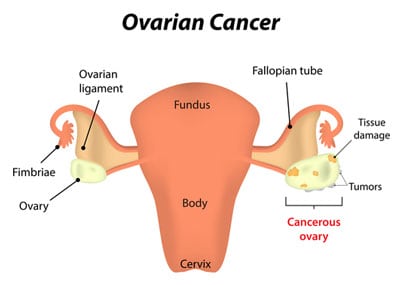
Surgery for ovarian cancer has 2 main goals. The first goal is to stage the cancer − to see how far the cancer has spread from the ovary. Usually this means removing the uterus (this operation is called a hysterectomy), along with both ovaries and fallopian tubes (this is called a bilateral salpingo-oophorectomy or BSO). In addition, the omentum is also removed (an omentectomy). The omentum is a layer of fatty tissue that covers the abdominal contents like an apron, and ovarian cancer sometimes spreads to this tissue. Some lymph nodes in the pelvis and abdomen are biopsied (taken out to see if the cancer has spread from the ovary).
If there is fluid in the pelvis or abdominal cavity, it will also be removed for analysis. The surgeon may “wash” the abdominal cavity with salt water (saline) and send that fluid for analysis. He or she may also remove tissue samples from different areas inside the abdomen and pelvis. All the tissue and fluid samples taken during the operation are sent to a lab to be examined for cancer cells. Staging is very important because ovarian cancers at different stages are treated differently. If the staging isn’t done correctly, the doctor may not be able to decide on the best treatment.
DEBULKING
The second goal of surgery for ovarian cancer is debulking or cytoreductive surgery. Debulking is important in any patient with ovarian cancer that has already spread widely throughout the abdomen at the time of surgery. The aim of debulking surgery is to leave behind no tumors larger than 1 cm. This is called optimally debulked. Patients whose tumors have been optimally debulked, have a better outlook than those left with larger tumors after surgery (called sub-optimally debulked).
Sometimes the surgeon will need to remove a piece of colon to debulk the cancer properly. In some cases, a piece of colon is removed and then the 2 ends that remain are sewn back together. In other cases, though, the ends can’t be sewn back together right away. Instead, the top end of the colon is attached to an opening (stoma) in the skin of the abdomen to allow body wastes to get out. This is known as a colostomy. Most often, this is only temporary, and the ends of the colon can be reattached later in another operation.
Debulking surgery might also mean removing a piece of the bladder. If this occurs, a catheter (to empty the bladder) will be placed during surgery. This will be left in place until the bladder recovers enough to be able to empty on its own. Then, the catheter can be removed.
Debulking may also require removing the spleen and/or the gallbladder, as well as part of the stomach, liver, and/or pancreas. If both ovaries and/or the uterus are removed, you will not be able to become pregnant. It also means that you will go into menopause if you haven’t done so already. Most women will stay in the hospital for 3 to 7 days after the operation and can resume their usual activities within 4 to 6 weeks.
Robotic surgery, or robot-assisted surgery, allows doctors to perform many types of complex procedures with more precision, flexibility and control than is possible with conventional techniques. From a console in the operating room, the surgeon views the internal organs through a 3D monitor and controls robotic arms inserted into the abdomen using ‘masters’ which are similar to joysticks. Robotic surgery is usually associated with minimally invasive surgery — procedures performed through tiny incisions.
Robotic surgery isn’t an option for everyone. Talk with your doctor about the benefits and risks of robotic surgery and how it compares with other techniques, such as other types of minimally invasive surgery and conventional open surgery.
Reconstructive urology surgery can help patients with conditions such as birth defects, cancer, neurological disorders, female incontinence, strictures, scar tissue in the urinary tract organs, and pelvic floor prolapse including cystocele, rectocele, enterocele, and uterine decensus.
Reconstructive urology can also help repair traumatic injuries to the kidney, ureter, bladder, and genitals. Traumatic injuries are often associated with pelvic fractures that can happen as a result of things like motor vehicle accidents or falls, and can often lead to scar tissue formation in the urethra.
With a vaginal hysterectomy, the surgeon makes an incision inside and near the top of the vagina. The surgeon then reaches through this incision to cut and tie off the ligaments, blood vessels, and fallopian tubes. Once the uterus is cut free, it is removed through the vagina. The procedure normally takes one to two hours. Often, the patient can go home the same day return to normal activities takes about one to two weeks.

Since the uterus is removed through the vagina, a vaginal hysterectomy is appropriate only for conditions in which the uterus is not too large, and in which the whole abdomen does not require examination using a more extensive surgical procedure. The advantages of this procedure are that it leaves no visible scar and is less painful. The disadvantage is that it is more difficult for the surgeon to see the uterus and surrounding tissue. Large fibroids sometimes cannot be removed using this technique.
Vaginal hysterectomy is the preferred route when it is an appropriate option. The advantages of vaginal hysterectomy include:
- Less pain and less risk of infection
- Faster recovery, often going home the same day and quick return to normal activities
- No visible scar
Research has shown that most ovarian cancer starts as a few undetectable cancer cells in a fallopian tube. The Remove Tubes Alliance (RTA) is a group of doctors committed to providing you easy access to local surgeons who will join any routine abdominal operation to also perform an elective procedure to remove your fallopian tubes.

Research has shown this simple surgery can help prevent up to 70% of ovarian cancer. The steps are simple and assume you have no plans for future pregnancy: as you begin planning your abdominal surgery, review the RTA doctors who have privileges at your hospital and select one.
Contact that RTA surgeon for your pre-surgery consult date, sterilization consent completion, and payment for the office visit and surgery. Payment is required as most insurances will not authorize the prophylactic removal of fallopian tubes. Your RTA doctor will keep coordinated with your abdominal surgeon (they have privileges at the same hospital) and will attend your surgery and preform the Salpingectomy.
vNOTES (vaginal natural orifice transluminal endoscopic surgery) is an advanced minimally
invasive surgical technique that eliminates the need for your surgeon to make incisions in your
abdomen to perform the surgery. Only a few of the highest volume surgeons in the country are
trained in this state-of-the-art technique. Imagine a hysterectomy without any visible scars, less
discomfort, and faster recovery than conventional laparoscopic or robotic surgery.
To learn more: https://www.appliedmedical.com/vnotes
Bay Area Gynecology Oncology specializes in pelvic surgery, vaginal surgery, laparotomy, and other surgical services throughout San Jose, Fremont, Santa Cruz, Los Gatos, Mountain View, Salinas, Carmel, and surrounding CA communities.
Contact Us
If you would like to reach us outside of our standard operating hours, please use the form below or call us at 408-827-4274 to be connected with the doctor on call.
Office Hours
Campbell
Mon-Fri: 8:00 AM - 5:00 PM
